What are depression symptoms?
Common signs include persistent low mood, loss of interest or pleasure, fatigue, sleep and appetite changes, feelings of worthlessness or guilt, trouble concentrating, slowed or agitated movement, and thoughts of death or self-harm. If these last most days for two weeks or more, consider screening and professional help.
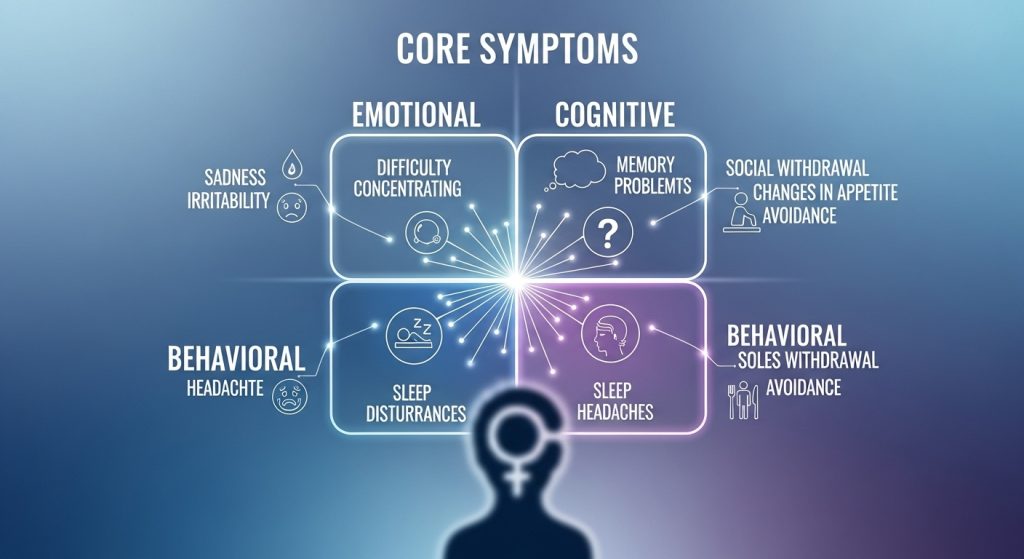
Table of Contents
- What depression feels like
- Core symptoms (emotional, cognitive, physical, behavioral)
- Depression vs. sadness (quick compare)
- Causes & risk factors
- Screening & diagnosis
- What you can do today
- Evidence-based treatments
- Lifestyle supports that actually help
- When to seek professional help
- Resources (US & Europe)
- Frequently asked questions
- About our medical review & references
- Appendix: Schema markup (JSON-LD)
What Depression Feels Like
Depression is more than feeling sad after a tough day. People often describe it as a heavy, empty, or numb state that blunts motivation and enjoyment. Getting started feels unusually hard; everyday tasks (emails, showers, meals) can seem overwhelming. It can also appear mainly in the body—fatigue, aches, and sleep changes—without obvious sadness.

Core Symptoms
Most clinicians group depression symptoms into four buckets. You don’t need every symptom to have depression, but patterns that persist for two weeks or longer and interfere with life warrant attention.
Emotional
- Persistent low mood, emptiness, or numbness
- Loss of interest or pleasure (anhedonia), even in favorite activities
- Irritability, tearfulness, or feelings of hopelessness
Cognitive
- Difficulty concentrating, remembering, or making decisions
- Negative or self-critical thoughts; excessive guilt or shame
- Recurrent thoughts of death or self-harm (seek urgent help)

Physical
- Low energy or unusual fatigue
- Sleep changes (insomnia, early-morning waking, or oversleeping)
- Appetite or weight changes; slowed movement or, sometimes, agitation
- Headaches, muscle aches, or digestive issues without clear medical cause

Behavioral & Social
- Withdrawing from friends, family, or activities
- Falling behind on routine tasks (work, school, household)
- Increased alcohol or substance use to cope
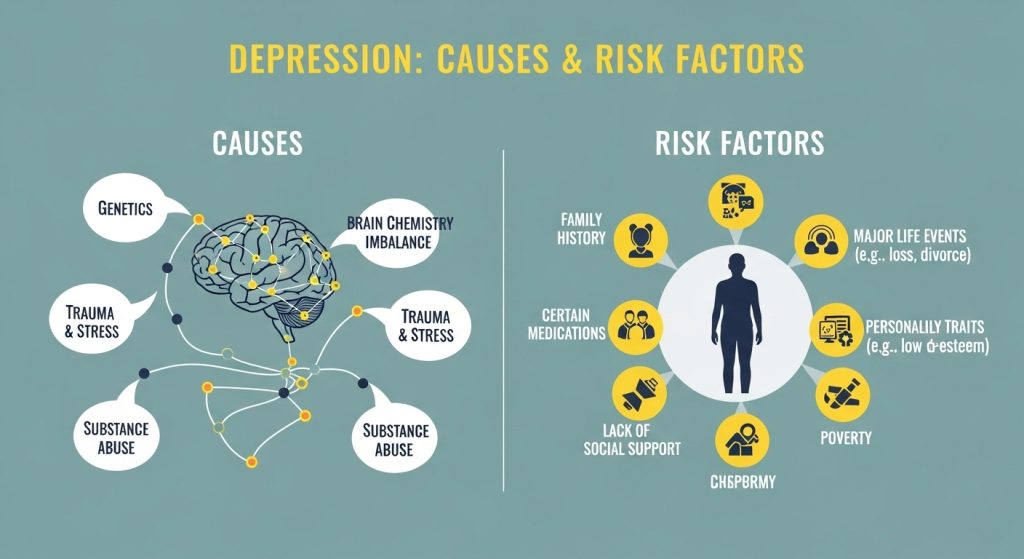
Causes & Risk Factors
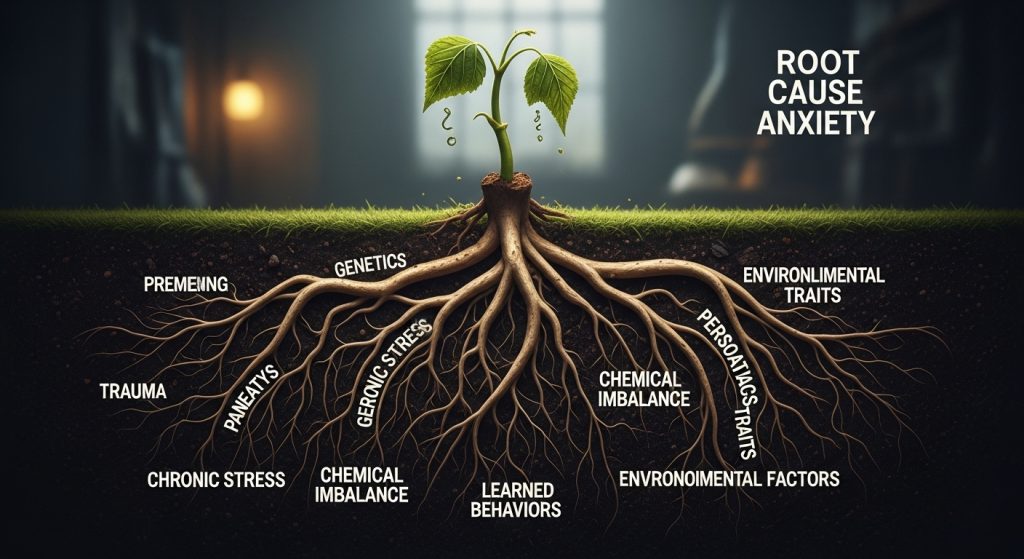
Depression seldom has a single cause. Common contributors include biology (genetic vulnerability; neurotransmitter and hormonal changes), psychology (unhelpful thought patterns; perfectionism; low coping skills), environment (trauma, grief, discrimination, financial/relationship stress, isolation), and medical/lifestyle factors (chronic illness, thyroid issues; poor sleep; inactivity; heavy alcohol/substance use). Protective factors—supportive relationships, routine, purpose, healthy sleep, and problem-solving skills—buffer against episodes and aid recovery.

Screening & Diagnosis
If the list above resonates, consider a brief, confidential screening. A common tool is the PHQ‑9, which scores symptom frequency over the last two weeks. Screening is not a diagnosis but helps you decide whether to reach out. A clinician (e.g., primary care, psychologist, or psychiatrist) will rule out medical causes and discuss treatment options.

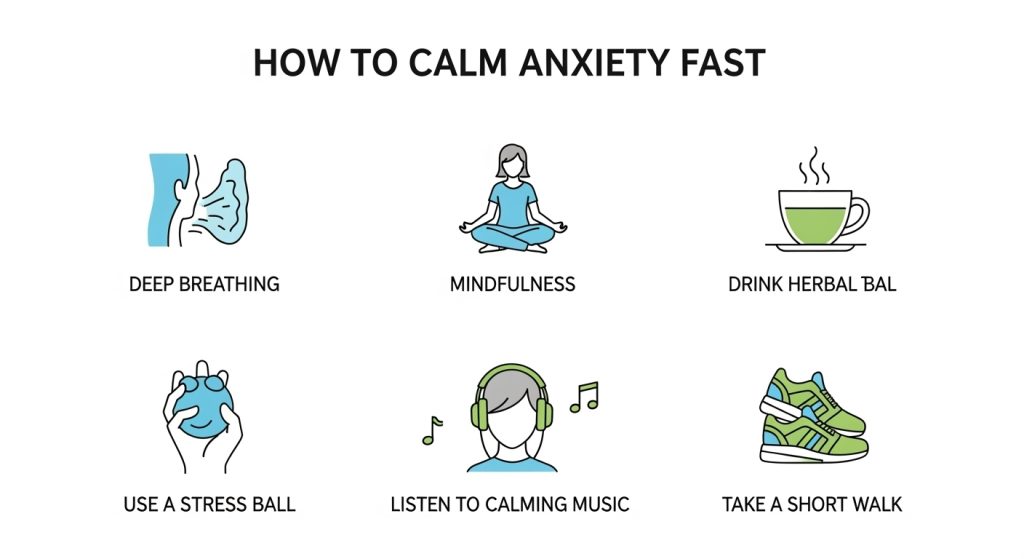
What You Can Do Today (5‑Minute Wins)
- Name it: Write down 3 emotions you feel and 1 trigger. Labeling reduces intensity.
- Behavioral activation micro‑task: Choose a five‑minute activity (shower, open blinds, step outside) and do it now.
- Breathing reset: Inhale 4, hold 2, exhale 6. Repeat 6 times.
- Connection nudge: Send a “thinking of you” text or voice note.
- Fuel & water: If you haven’t eaten or hydrated, do both before making big decisions.

Evidence‑Based Treatments
Good care is individualized. Many people benefit from a combination of therapy, skills practice, and (when appropriate) medication.
Psychotherapies
- CBT (Cognitive Behavioral Therapy): Tools to challenge unhelpful thoughts and increase healthy behaviors.
- Behavioral Activation (BA): Structured steps to rebuild routine, pleasure, and a sense of accomplishment.
- IPT (Interpersonal Therapy): Focuses on relationships, role transitions, and grief.
- Mindfulness‑based therapies: Skills for attention, acceptance, and relapse prevention.
Medication
SSRIs and SNRIs are common first‑line options for moderate to severe depression. A prescriber will discuss benefits, side effects, and how medication pairs with therapy. Give any medication an adequate trial (usually several weeks) and avoid stopping abruptly without guidance. You can also visit this article to read about Anxiety Symptoms.
Other Options (case‑by‑case)
- Augmentation strategies when a first‑line medication is partially effective
- Neuromodulation (e.g., TMS) for treatment‑resistant cases
- Collaborative care models integrating primary care and mental health
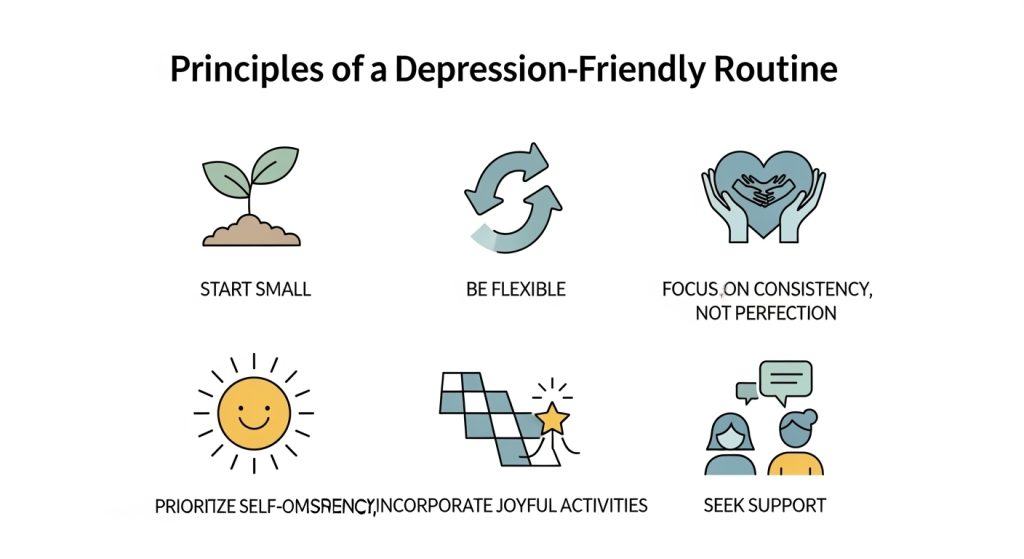
Lifestyle Supports That Actually Help
- Sleep: Fixed bed/wake times; limit screens 60 minutes before bed; dark, cool room.
- Movement: Gentle activity (e.g., 10–20 minutes walking) improves mood and energy.
- Nutrition: Regular, balanced meals stabilize thinking and energy; limit heavy alcohol.
- Routine & boundaries: Plan breaks; say no when capacity is full; add buffer time around commitments.
- Purpose & pleasure: Schedule one small meaningful or enjoyable activity daily.
- Social connection: Join a group, class, or peer support meeting.
When to Seek Professional Help
Book an appointment if symptoms persist most days for two weeks, you’re struggling at work/school/home, or safety is a concern. Screening can be a first step: try our quick, confidential screening tools (/screening-tools), then use Find a Therapist (/find-a-therapist) to book care. If you’re worried about immediate safety, use the crisis options at the top of this page.
Resources (US & Europe)
- United States: 988 Suicide & Crisis Lifeline (https://988lifeline.org/) • NIMH Mental Health Topics (https://www.nimh.nih.gov/health/topics)
- Europe/UK: Emergency number 112 (EU information page) • Samaritans 116 123 (https://www.samaritans.org/how-we-can-help/contact-samaritan/talk-us-phone/)
- Global directory: Find A Helpline (https://findahelpline.com/)
FAQs
What are the first signs of depression?
Loss of interest or pleasure, persistent low mood, unusual fatigue, and sleep/appetite changes are common early signs.
How do I know if it’s depression or just stress?
Stress usually improves with rest and coping. Depression tends to persist most days for two or more weeks and affects functioning.
Can depression be mostly physical?
Yes, some people notice fatigue, aches, or sleep/appetite changes more than sadness.
Do I always need medication?
No. Many benefit from therapy alone, especially for mild to moderate cases. For moderate to severe cases, medication plus therapy often helps most.
How long does recovery take?
It varies. Many people see improvements within weeks of consistent therapy, skills practice, and/or medication. Relapse prevention is part of good care.
